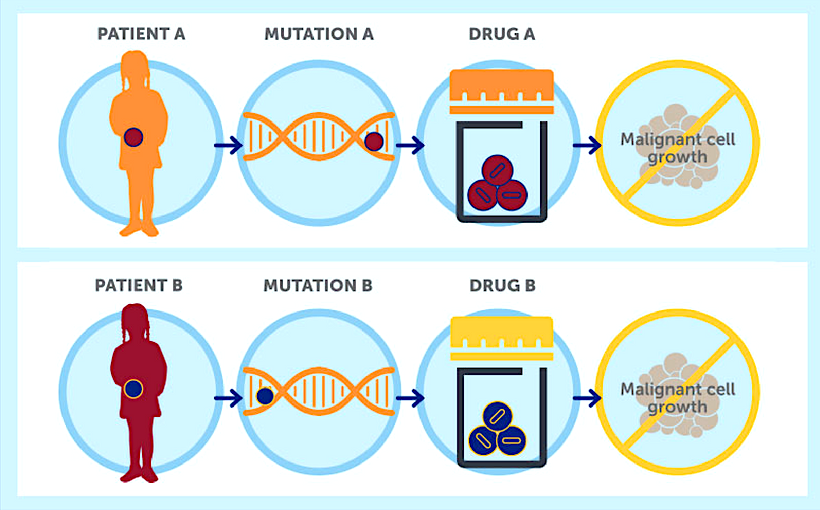
The way we treat cancer is rapidly changing. We know that individual cancers cause different genetic changes and that new drugs targeting these differences could help improve treatment. This approach is known as precision medicine. In addition, there are treatments using the immune system to attack the cancer, known as immunotherapy. The number of these new treatments have grown hugely over the past few years. In 2018 alone, they accounted for over 90% of the new cancer drugs being developed. These new treatments are also often associated with hefty price tags. For example, immunotherapy as a course of treatment for advanced lung cancer, can cost over £80,000.
Used alongside these new treatments are specific biomarker tests, which help determine if the cancer is likely to respond to these drugs. Doctors use this information to guide decision making so that in theory, the right patients, who will benefit the most from these drugs, receive them. Without biomarker testing it may be impossible to access these drugs or use them appropriately.
Sounds great, so what’s the catch?
Unfortunately, we know with traditional cancer treatments (surgery, chemotherapy and radiotherapy), that access is not always decided based on the patients’ needs. There are many complex reasons why this might be - and having a lower socio-economic status is one of them. Socio-economic status means your individual or family’s social and economic standing relative to others. It is measured using factors such as income, education and your job. Socio-economic reasons may impact the number of other health conditions a patient has, their ability to request help or even the conversation they have with a doctor. All of which can affect the treatments they receive and the outcomes from therapy. What we don’t know yet is whether the socio-economic differences we see in traditional cancer treatments are also seen with both biomarker testing and the delivery of precision medicines and immunotherapies described above.
Why is this work important?
The NHS was set up on the idea that treatment should be provided to all on the basis of clinical need. We don’t expect that our level of education, the amount of money in our bank accounts or the power associated with our jobs will affect our access to treatment compared to another patient diagnosed with the same cancer at the same stage and with the same prognosis. Yet if these newer treatments can improve cancer outcomes (for example by increasing tumour responses, minimising side effects and improving survival), socio-economic status should not be a factor in determining access. We already know that socio-economic differences are present in cancer survival, but this could be exacerbated if patients with lower socio-economic status are restricted from biomarker testing and access to new therapies, so we need to assess the size of this problem (if any).
What did we do about it?
To investigate this question, we carried out a new systematic review (reviewing the available high quality research evidence) using 58 previous studies showing information on over 1 million patients. Newer cancer drug access was compared between patients with a low to a high socio-economic status. The review looked at 7 cancers, 5 biomarker tests and 11 cancer therapies. The evidence showed that patients with a lower socio-economic status were 17% less likely to receive newer cancer treatments when compared to those patients with a higher socio-economic status. However, the strength of these differences did vary with cancer type, and were clearest in lung cancer. Similar differences were also seen in access to biomarker testing (often seen as a precondition for new cancer drug access).
Can we trust this evidence?
As 42 of the 58 studies were from the USA, more work is needed using UK data to see if similar patterns are observed here. Also, as studies used different measures of socio-economic status (i.e. some income, others education etc.), we need to be careful making conclusions in case the choice of measure used affects the strength of the findings.
What next?
Our review shows that we need more research questioning why factors such as income and education could still be affecting treatment access when clinical decisions should be guided by the patient and tumour genetics. It is important that whilst continuing the important research in developing new precision medicine and immunotherapies, we work to ensure fair access to all patients regardless of socio-economic differences.
Take home points
- Cancer treatment is now guided by genetics and new cancer drugs can help personalise care.
- Having a low socio-economic status can reduce the likelihood of receiving a newer cancer drug and the test linked to your eligibility for the new drug.
- We need more UK based research to investigate these differences, to ensure fair access and reduce differences in cancer outcomes.

No comments:
Post a Comment