 |
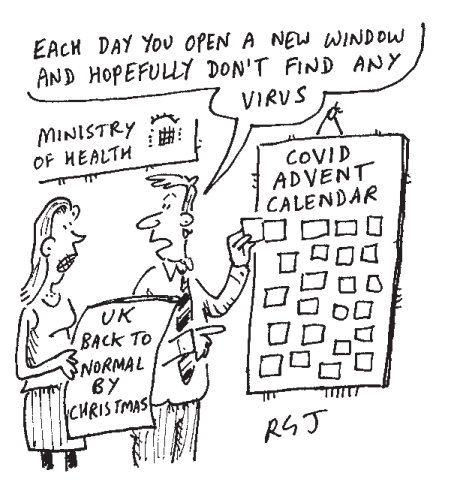
| Image credit: The Spectator magazine and the illustrator Richard Jolley |
In keeping with the spirit of the season, my own advent calendar of symptoms has popped open several new windows this week, most notably ‘pins and needles’ and joint pains. Both have arrived on top of the commonly experienced and more worrying long-term chest pains (eight months in my case) and irregular erratic heart rate (managing over 200bpm at rest on one occasion (the normal range for healthy adults is between 60 and 100 bpm). This combined with a rogue ECG readout (Electrocardiograms test the heart's rhythm and electrical activity) in a local A&E department earned me an unscheduled two-night stay in hospital six weeks ago. Seemingly intractable tinnitus has become another constant ‘companion’.
Thanks to my local NHS Hospital, my symptoms were comprehensively investigated and I continue on the ‘recovery’ journey - if recovery is not too optimistic a label. Recent findings from several studies on the longer term complications of the disease have however made for uncomfortable reading, all the more so for being carried out in people whose symptoms had generally not been particularly severe.
In the first of these, a Frankfurt based cardiac MRI study(3) recruited 100 cases of non-hospitalised patients in whom 78% were found to have disruption to heart muscle function and 60% ongoing heart tissue inflammation. Given that the number of ‘milder’ cases will always inevitably far outweigh the numbers hospitalised or who tragically do not survive, the sheer scale of the potential public health disease and premature death burden (if heart health is undermined), begins to look very concerning(4).
In the first of these, a Frankfurt based cardiac MRI study(3) recruited 100 cases of non-hospitalised patients in whom 78% were found to have disruption to heart muscle function and 60% ongoing heart tissue inflammation. Given that the number of ‘milder’ cases will always inevitably far outweigh the numbers hospitalised or who tragically do not survive, the sheer scale of the potential public health disease and premature death burden (if heart health is undermined), begins to look very concerning(4).
 |
initial symptoms (mask displaced to drink) |
Perhaps more worrying still, ‘long covid’ does not seem to restrict its attentions to the heart and lungs, with another study finding evidence of multiple organ damage in 201 people with a largely mild course of disease, 70% of whom had damage in one or more organs, including kidneys (12%), liver (10%), pancreas (17%) and spleen (6%), as well as heart (32%) and lungs (33%) four months after initial symptoms(5).
Adding further to this complex picture was a news release about a study this week of ten patients at Oxford University in which a novel scanning technique was used to successfully identify damage not picked up by conventional scans(6). Eight of the ten patients still experiencing shortness of breath three months after infection (none severe enough to be hospitalised), had evidence of hidden lung damage. The new technique will now be repeated with a much larger sample.
These worrying findings about potential long-term damage are already prompting some big-picture questions: What proportion of people who only had very mild disease will go on to develop organ damage? Proportions like 60% and 70% could potentially translate into a staggering public health disease burden with very substantial implications for health services. Devastating though the considerable loss of life has been, the eventual population impact clearly has the potential to be far greater(4).
As always with such matters however, it is never especially helpful or productive to dwell too long on ‘worst case scenarios’. For my own part, I am fortunate to be in a non-physically demanding job with an understanding employer. The prospect of accommodating such an unwelcome guest as long covid in a physically strenuous job or on a zero hours contract (or both) does not bear thinking about. Long covid clearly has the potential to further exacerbate the substantial inequalities in health and social outcomes that have so clearly characterised the current pandemic.
Significant unanswered questions also remain around which population groups are most likely to be affected by long covid: do they correspond for instance to those most at risk of not surviving? Early indications are that this might not be the case, at least as far as age or gender is concerned: while there has been no systematic population prevalence study, long covid seems to disproportionately affect younger and middle-aged adults, and females over males. For some this latter observation lends credence to long covid being ‘auto-immune’ in origin since women tend to be at higher risk of such diseases (lupus and rheumatoid arthritis being two prominent examples).
Would vaccination be helpful for those affected? Or might it be dangerous given the likely involvement of a misdirected immune response as the basis for the condition? In these respects it’s extremely encouraging that long covid is receiving high level research attention that seems to be already helping to unravel its impact, causes and effects. Such efforts may ultimately be at least as valuable as the impressive progress with vaccine development.
Returning to the advent calendar of the title, the wonderful thing about advent is that there is a season of joy and festivity at the end of a dark midwinter month. Here’s hoping that there is an end in sight also for the many afflicted by long covid.
References:
- Paul Garner on long haul covid-19—Don’t try to dominate this virus, accommodate it - The BMJ September 4, 2020. https://blogs.bmj.com/bmj/2020/09/04/paul-garner-on-long-haul-covid-19-dont-try-and-dominate-this-virus-accommodate-it/
- Paul Garner: Covid-19 and fatigue—a game of snakes and ladders - The BMJ May 19 2020. https://blogs.bmj.com/bmj/2020/05/19/paul-garner-covid-19-and-fatigue-a-game-of-snakes-and-ladders/
- Puntmann VO, Carerj ML, Wieters I, et al. Outcomes of cardiovascular magnetic resonance imaging in patients recently recovered from coronavirus disease 2019 (COVID-19). JAMA Cardiol. Published online July 27, 2020. doi:10.1001/jamacardio.2020.3557
- Mooney, JD, Ling J. Long covid: a potential longer term morbidity time bomb?: Rapid response to: BMJ 2020; 371. doi.org/10.1136/bmj.m4470
- Dennis A, Wamil M, Kapur S, Alberts J, Badley AD. Multi-organ impairment in low-risk individuals with long COVID. https://www.medrxiv.org/content/10.1101/2020.10.14.20212555v1.full.pdf
- BBC News: Covid-19: Lung damage 'identified' in study: 1st Dec 2020 https://www.bbc.co.uk/news/health-55017301
Acknowledgement to high profile fellow awareness raisers of #LongCovid:
Professor Paul Garner: Liverpool School of Tropical Medicine: @PaulGarnerWoof
Dr Nisreen Alwan: University of Southampton @Dr2NisreenAlwan


No comments:
Post a Comment